What a journey Cullen’s creation and journey into this world truly was. Now that he is five months old, it really is time to sit and process the journey, and share with those who want to hear.
I found out I was pregnant with Cullen the afternoon on January 29th, and I was incredibly shocked. For those that don’t know, I have dealt with chronic pain issues since Aibhlinn was born. I spent her first year of life thinking I had destroyed my body with bed rest, and I just needed to work on strength to get better. By time she was a year and a half, I started having pain episodes that utterly paralyzed me for days. I was finally diagnosed with hip dysplasia, which apparently can get worse after pregnancies. In looking at all the options to best help, I decided to have a surgery in December that was consider less invasive than others to hopefully help my hip. You are told you should not get pregnant for 12-18 months, which I assumed would be no big deal.
So my huge surprise to be 7 weeks post op and to find out I was pregnant was a huge shock. The day before finding out, I threw up both doses of this multi vitamin I took. Something in my mind said maybe amazon a pregnancy test, but it is probably nothing. I really did not think I was pregnant.

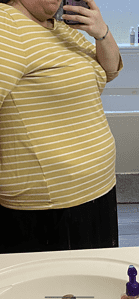
Definitely pregnant!
The test came in around lunch time on the 29th of January. I took it, and it was positive. Since my history is long with recurrent miscarriages and it was too late to see my reproductive endocrinologist, I grabbed a lab form from my office and ran to Quest to run labs on myself. I was pleasantly surprised to see “high” progesterone levels for myself that day without supplementation, and got in with my specialist the next day for labs and prescriptions to start progesterone and Lovenox to help me maintain the pregnancy.
My first HCG came back at 49, which means a minute pregnant and I am already throwing up. It’s incredible how sensitive my body is to pregnancy. I did not know the half of it yet though!
I made a point to run to Sprouts for some new supplements so that I could catch up on getting nutrition in. I have been prone to having a lot of food aversions and nausea in my pregnancies, with each one getting progressively worse, but I was not mentally prepared for how hard this pregnancy was going to be. I remember exactly the last day I could handle choking down the smoothie of vitamins at 7 weeks when I threw it all up in the emesis bag in the car while going to pick up the oldest from an event.
The food aversions were insane. So much worse than I remembered. I literally could only eat or drink what crossed my mind as okay to eat or drink. I tried a couple other vitamins, but they were all a bust, and if I forced myself to take them anyway, I would throw them up. So I spent most of my pregnancy taking zero supplements which was a first for me.

My first IV bag of fluids of many in pregnancy.
I always try to avoid medications as much as I can because I am nervous about the effects they will have on the developing baby, but as 9 weeks neared, I was starting to feel desperate. I was so sick so much of the time and it was hard. I finally tried my oral zofran prescription, and I was sorely disappointed to find that it did nothing for me. It did not control my nausea and it did not control my vomiting.
It was a Saturday evening in my 9th week that I had the realization that I was dehydrated. I may be a midwife, but I am a terrible midwife to myself. I had an overdue client I was waiting to go into labor, and was a bit concerned how I would handle being on my feet with how I was feeling. I decided to go into urgent care for some IV fluids. The on call doctor was great, and even though it took a couple tries because I have terrible veins and apparently was quite dehydrated, he got me and gave me a bag of fluids. When I was checking out, I saw the diagnosis code he gave me was “Hyperemesis Gravidarum”, and I was thinking there is no way. That’s not me. I am just in a weird place for some reason, and it will pass. Because the second trimester is the glorious trimester and it MUST get better, right?
I left with a prescription for phenergan, but it was too late in the evening to fill it. I threw up before even hitting the high way on my way home, totally bummed that I was already throwing up.

One of my weekly vitamin bag infusions.
I got the prescription filled the next day, and tried one. I never took another one again. The drowsiness hit me hard and fast. I texted a midwife friend quickly what I took and begged her to cover for me if one of my clients delivered before the side effects of the medication wore off. So phenergan, in my opinion, works because it makes you sleep so much you can’t be awake to be miserable. I was so out of it for almost 24 hours, waking only out of starvation or to vomit. It was awful!
In the continual mind game of finding ways to cope, I remembered that clients who I sent for vitamin therapy raved about how much better they felt for a few days following their infusion. It took some work, but I found someone who would come to my house once a week to give me a Myles Cocktail, and I was sure this would be magical.
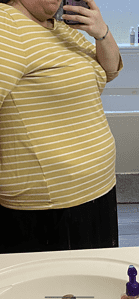
The first signs of a baby bump.
The weekly IV infusions proved to be ineffective unfortunately. In hindsight, I am sure it was helping me skirt by in dehydration land for a short period of time.
In my 13th week, I was unable to tolerate water any longer. It had been a slow progression as I went from drinking room temperature water, to only handling cold water at 8 weeks, to now being unable to tolerate any water. I could tolerate ice, so my awesome husband would throw ice from Buccee’s into the Vitamix and I would try to choke down ice through out the day.

The in home make shift IV holder.
My 14th week was the start of a horrible spiral that took weeks to recover from. I was suppose to see clients this particular day, but I was in bad shape. It started when I woke in the night that I felt like I was on a cruise ship, and the boat was really rocking. By morning, I was so dizzy that I couldn’t safely get out of bed alone. I was so confused by why I was feeling so bad. I messaged my midwife friend who was my own preceptor and my midwife for Aibhlinn. She recommended I take my blood pressure, pulse, and blood sugar. The end thought after taking my vitals was that I was severely dehydrated. My midwife wanted to admit me in the hospital for a couple of days for continual fluids, but I refused.

So many IVs.
I did not want to start the cycle of being admitted, and with the start of COVID, I would be completely separated from my husband and children, and I didn’t want that. In reflection, in these horrible moments of severe dehydration from vomiting 10 or 20 times a day, I wasn’t always able to think the most clearly and make the best of decisions. Since I wouldn’t go in, my midwife came over that evening to start an IV. This ended up being a very complicated ordeal. She attempted six times to start an IV, and each time she would get flash and my crappy, dehydrated veins would blow. Finally, the last attempt resulted in a vein that wanted to cooperate. We ran fluids continuously, but 24 hours in, my IV failed and that was that. Every time I had IV fluids during my pregnancy (which was multiple times), my veins would not last long enough to help me get caught up.

Also… so many blown veins.
By time I was 17 weeks, I literally felt like I was going to go out of my mind if I couldn’t get a break from relentless, debilitating nausea, vomiting 10-20 times a day, dry heaving double or triple that a day, etc. My doula suggested that I schedule an appointment with Dr Gei for management of my Hyperemesis. I got in fairly quickly, where Dr Gei couldn’t even understand how I held off so long. He immediately ordered me a zofran pump to start, and within 48 hours the home health nurse was at my house getting the pump set up.

The fancy zofran pump.
Although not perfection, the zofran pump dramatically minimized my vomiting episodes down to 1-3 most days. It did not help my nausea or food aversions unfortunately, but to skirt by hydration wise and minimal vomiting was a win.

The beloved frosted coffee from CFA.
Eating was an ordeal my entire pregnancy. I had very severe food aversions, and could only eat what sounded good to me in that moment. My longest running safe foods were sour dough bread from the farmers market with Kerry gold butter (sometimes I could handle it with cheese or bacon), 7oz cans of coke (it literally had to be the 7oz cans, no other form), cheese (but this would dramatically jump forms of what flavors or presentations of cheese I could tolerate), and Frappuccino’s (but this would change all the time on what place I could handle one from). Basically, I was ridiculous!

He was definitely growing in there! Around 22 weeks.
One weird thing that comes with Hyperemesis is ptyalism, otherwise known as excessive salivation. It’s totally disgusting, and was out of control. It literally would make me gag or even vomit. The taste would make me sick. I learned in some support groups on social media how to manage, so I got some awesome pointers like sour candy and cinnamon candy to help.
Probably my best time frame of pregnancy was mid May through mid July. The veil of feeling like death was not so heavy during this time frame, and I was so thankful.

3D Ultrasound
Just like 29 weeks and on brought so much drama in my last pregnancy, it sure brought some utter chaos in this one. The day I turned 29 weeks, I was feeling pretty decent. I was so impressed with myself that I got two entire protein shakes down which was an accomplishment. My MFM had wanted me to drink three a day, and I was lucky to choke down one a day. I knew increasing my protein intake was significant for baby’s growth in the third trimester, and I though maybe for once my body was co-operating!
NOT! Because why would it want to do that!? That night I went to bed feeling a funky pain in my “hip”. Since I have hip dysplasia and arthritis in my right hip, I just thought I did something funky to my hip to cause the weird pain and didn’t think any more of it. I was finally able to get to sleep, and found myself awake the next morning around 430am, the pain worse but I was also having contractions.
Some time passed, and I decided to try a bath because the contractions were getting more uncomfortable. The bath did not help. I wasn’t aware of the weird hip pain anymore, and only aware of how awful the contractions were starting to feel.
As the morning progressed, things got worse. I started having horrible chills, and was making Christopher take my temperature over and over again. Contractions were so painful, I remember at one point thinking either a 29 week baby was going to plop out on the bed or I was dying, I only felt this bad during transition. I wasn’t able to communicate well to Christopher, so he reached out to my midwife, Rowan, for guidance. She got him connected to calling Dr Gei, who told him to bring me into the office.
I must have looked a lot like death because during subsequent appointments, everyone commented on how much better I looked after this day. I was so weak, I couldn’t walk without support. It was awful. Ultrasound showed my cervix dramatically shorter since my previous ultrasound three days earlier. My blood pressure was 86/48 and pulse 135 in the office. Dr Gei said he was sending me across the way to be admitted for fluids, labs, and observation.

Goodbye zofran pump!
I was in the hospital for three days. Since I had cervical change happening, I received steroid injections for the baby’s lungs to be safe. My labs came back showing I had a minor kidney infection, and was narrowly away from kidney failure. Thank you, Hyperemesis!

My maternity pictures taken at 32 weeks.
I spent the remaining weeks feeling pretty miserable. The zofran pump wasn’t working anymore, so Dr Gei stopped it the beginning of August. I was exhausted, sick, and miserable. The third trimester was definitely amplifying all the fun feelings all over again. The plus side of things is that overall, this pregnancy the preterm labor fun wasn’t as apparent as it was with Aibhlinn or even the boys. When I had contractions, they weren’t as frequent but they were definitely very strong. I assumed this was the case since I was so sick I had no choice but to rest most of the time.

Aibhlinn became an expert at fake vomiting.
This whole pregnancy I envisioned and imagined a home birth. I couldn’t “see” Cullen being born anywhere else. I had a goal set for myself that if I stayed pregnant until September 1st, I would have him at home, and would not need my back up hospital plan.
I was so thankful to make it to September 1st! We unpacked the hospital bags, threw away the hospital birth plans (because I am a multip, and would never have a reason to transfer at this point aside from an emergency, right!?), and got the last minute home birth supplies we needed.

Another one of my favorite maternity pictures.
While waiting for the baby to come, we were deep in the process of getting our affiliation with our mission sending organization, New International. Part of that process is a one on one interview, which I was stressed about getting complete before Cullen was born. Christopher’s interview was complete almost two weeks before I heard from anyone about mine, and I was getting antsy!
The evening of September 2nd, I received an email from the lady who would do mine who by the grace of God had availability the next morning for my interview. So Thursday, September 3rd, I completed my interview around 11am, and Christopher and I then went to lunch. During lunch, I started realizing that I was having to focus on contractions that were coming every five minutes or so. These contractions stayed all day long, making it clear that I needed that interview done before my body was like, “okay, we can have a baby now.”
Sleep was very rough that night as the contractions were strong enough to affect sleep but weren’t active labor.
I felt awful all day, Friday, September 4th. We decided to have my in-laws come up to watch the kids so that Christopher could be with me. My Hyperemesis symptoms were horrible all day, and I could barely handle being out of bed, while also having contractions. It was awful, and as the day progressed, I felt more discouraged because I “needed” to be done in every way. This pregnancy challenged me in every capacity, and I often didn’t want to do it anymore, but now I really didn’t need to do it anymore if labor would just pick up!

Sara starting my IV fluids.
My friend and planned birth assistant, Sara, came over late afternoon to go ahead and get my IV started. This was important to me because I was feeling so crummy and felt I might need some fluids and labor had to be on the horizon. I had early labor for several days before I had Aibhlinn which I feel like contributed to my postpartum hemorrhage after her birth, and I was not going to do that again.
I messaged my midwife, Rowan, that evening and made the plan that if I didn’t call the team over in active labor overnight, that I wanted my water broke the next morning and get this show on the road. Again, I was DONE.

Checking on baby.
It was another night of horrible sleep that frustrated me because I knew I wanted sleep for labor and that it would be my last nights of sleep not being interrupted.
I was happy to wake up feeling more clear headed and with some energy that morning. I was still contracting, and decided that I was going out for a walk. So Gideon and I headed outside at 6am to walk the short distance around our end of the neighborhood to see if things would amp up.

Side lying release with my doula, Jessica.
I texted Rowan at 8am confirming that I did indeed want my water broken. She arrived at 945, and I was so grateful to see her. Her arriving early meant I should have a baby by dinner, and everyone back home before bed time, and I wouldn’t be inconveniencing anyone. Should being the word I should have thought more about with this journey!

When labor was happy and progressing.
Rowan arrived around 945am, and took my vitals and listened to baby before doing my exam. There was a snafu with breaking my water so we had a slight delay as Christopher had to run up to my office to get a hook to break my water since Rowan liked those better than the cots I had at the house. He was back by 1040, and my water was broken at 1045. I was 5cm dilated, 75% effaced, and baby was at a -2 station. This is roughly where I am every time my water is broken, and a baby follows in 4-6 hours. Once my water was broken, we notified everyone else to go ahead and come so that everyone was here with me since we expected things to get active fairly quickly.

The last hours of a baby bump.
By 12pm, my entire team had arrived. Sara flushed my IV and started my fluids. I made the decision to have an IV in labor early in my home birth planning after my hemorrhage with Aibhlinn and with the fact that I couldn’t hydrate well with Hyperemesis. I was happy to get the fluids started, and the stress of me having to keep the fluids up diminished.
I spent this time alternating between walking around my bedroom and sitting on the birth ball. It was a fun time chatting with my birth team, who I consider friends, between contractions.

Working on the birth ball.
Around 1pm, my doula, Jessica, suggested I get on the bed and do a side lying release to help with labor progression. The side lying release really changed things, and contractions were noticeably more intense after doing the release. That made me happy, as I was ready to meet this baby!
Nausea started to get awful, and I was so scared to spend my labor vomiting, so Sara administered my zofran in my IV to help. I am so happy that we stayed on the zofran in labor, because I never threw up this labor which is impressive. I was horribly nauseated and dry heaved, but no vomiting!

Aibhlinn visiting me in the birth pool.
Jessica did some massage work before suggesting I walk around the room again.
As 2pm came, my contractions were every 1.5-3 minutes, lasting about a minute long. Silas came in the room at some point, being his silly self. After I walked around the room, I got in exaggerated sims position in the bed, where Cullen started moving like crazy.

Christopher talking about his vests while I am eating cheese definitely brought on the laughter.
I was having a hard time staying in one position at this point, and was out of bed and alternating between the birth ball and walking around the room. It was decided I was going to get in the birth pool at 340pm, as contractions were strong and I was hoping to meet my baby in the next couple of hours.

I think this is one of my favorite pictures that Stephanie captured of my birth journey.
The pool felt great. I remember at one point it getting discussed about Christopher’s clothing selections and how he wears the same thing for a period of time before wearing some other style for a period of time. When I had Aibhlinn, he wore this vest that I gave him a hard time about, and I remember during one contraction him telling me he was given another vest that was in his office at the church, and I just lost it in laughter.

Rowan doing some work to help this boy come down.
Aibhlinn came in at one point to check on me, and she was so sweet about the pool. I was super nauseous, but they convinced me to eat a piece of Swiss cheese while in the pool since I had not eaten since 9am.
As a planner and a midwife, my brains wheels started going as we got closer to what ended up being two hours in the birth pool. My contractions were no different in the pool, and I was getting frustrated. He should be here by now, so why isn’t he?

Trying to slow dance this boy out of me during contractions.
I got on the bed, and alternated sides with contractions to see if we could help him rotate into a better position.
Rowan requested doing a cervical check at 630pm to assess progress and to see if could find a reason for the hold up. I was 7cm dilated, 75% effaced, and baby at a -1 station. Rowan said I had some scar tissue that she worked on during the exam. It was not fun to say the least!

I can feel the whole energy shift just looking at this picture. I was so defeated at this point.
Discouragement and frustration set in hard at this point. It’s now 7pm, the baby isn’t here yet, and it felt like there was no end in sight.
For the next two hours especially, I was trying to trouble shoot in my head. I was convinced at one point my hip dysplasia must have screwed up my pelvis and he was not able to come down. Rowan assured me my pelvis felt great and that was not the issue. At one point I noticed my contractions were coupling and figured his position must be awful, but everyone assured me he was anterior so then I blamed that he had to be acynclitic.

Lift and tucks by Mary.
During this time, Jessica had me moving. When Christopher could be in the room, she wanted us doing the “slow dancing” position during contractions to help keep things long and open. When my legs were tired, I would sit on the birth ball.
Around 9pm, I assumed labor wasn’t progressing because I couldn’t eat. So I angrily ate another piece of Swiss cheese, convinced I needed food for my body to have the energy to finish.

Walking laps in the kitchen and living room in the light of our fall tree.
During this time, I alternated the same old positions, getting frustrated with each contraction that passed because I knew things weren’t getting stronger. Around 11pm, I got in open knee chest where Rowan and Jessica worked on different parts of my pelvis to help the process. This happened routinely in my labor that they would work and massage on areas, throwing all the things at me to get to the finish line of this labor.

During the flying cowgirl.
I couldn’t handle being on my knees for a long time because of my dang hip, so we began to alternate side lying, with different people working on my pelvis. The room was dim, and my exhaustion was overtaking me, and I found myself dozing in between contractions.
As the new day was upon us, I realized I was becoming very hyper aware of my labor play list. When I made my play list, I really only expected to listen through it twice. When Pandora finished playing through my list, it would auto play music that was like my play list. I immediately knew when it did that, and would need someone to restart my play list right away, but at the same time get frustrated that it was having to be restarted AGAIN! I am also sure my entire birth team was tired of hearing my music, which I don’t blame them. I also was feeling emotional that everyone had been with me for over 12 hours at this point, and I knew they were tired, exhausted, and frustrated. They assured me they were fine, but I knew better. Because as a midwife, we all know late nights births and long births are exhausting, and I felt horrible that nothing was going the way I expected. I clearly have control problems.

And still in the flying cowgirl…
Right after midnight, Rowan had her birth assistant, Mary, do lift and tucks for ten contractions to see if that would help. Unfortunately, it did not help and was yet another frustration on the journey!
After the lift and tucks, my birth team convinced me to leave my room and make laps around my kitchen and living room. So Christopher helped push my IV pole while I slowly made laps, nausea becoming overwhelming.

Waiting for the birth pool to finish filling.
Rowan wanted to do an exam at 145am, and the information was less than ideal. Not only did I not progress, but I in fact had gone backwards and was having cervical swelling. Rowan mentioned that if I did not make progress in the next few hours, we would need to discuss transporting. I don’t remember what I said out loud, but I remember thinking internally, “Oh no we won’t be.”

Finally in the birth pool!
Apparently the whole transport talk was a big controversial topic that I wish I could have been a fly on the wall to hear. With it, Christopher did two things. First, he made a sign that said “Cullen, it’s your birthday” styled after The Office episode, and second he apparently threw together a suitcase for transport that I only found out days later because I couldn’t find a lot of my clothes.
I went to the bathroom after the exam, and was desperate for what I could do to make progress happen. I had been given what felt like hundreds of homeopathic remedies that clearly weren’t helping. I couldn’t handle herbs because of the taste. I prayed so hard that progress would happen and I would finally be done.

In between contractions.
Jessica put me in a position called the flying cowgirl that I was not familiar with, and had a hard time wrapping my head around how it would help. I was able to rest in between in this position, and every time I felt like I could get in a comfortable spot, Jessica would yank my legs back more!
I was in that position an hour, but in the moment there was no sense of time. I wasn’t always aware of what was going on around me. Contractions were changing. They were painful, my hips ached, there was pressure building every where with each contraction. I was aware at moments of Jessica working on my back behind me, and sometimes it was my husband next to me, holding my hands and praying over me, and sometimes it was Stephanie, my birth photographer.

I love this picture because I know it was when I was being intense wanting Rowan to be ready, and to tell me if he was coming.
Around 3am, I was encouraged to get out of the bed and make laps around the house. I was very emotional through out the last few hours, but even more so this last hour. The contractions were awful, and physically I knew this had to be transition, but mentally I wasn’t trusting my body would do the work anymore, and labor was completely awful at this point.
The laps around the kitchen and living room were agony, and I was so weak. It took all I had within me to keep one foot in front of the other, depending completely on my husband for support with each contraction. I hit a wall at one point where I felt flustered and said I can’t do walking anymore. I went back into the room and sat on the birth ball, crying with each contraction and leaning on my husband because I felt too weak. Contractions were 2-3 minutes, lasting 90 seconds at this point.

Praise God, he is finally here!
The team were actively warming the birth pool at this point, but I wasn’t aware. I remember sitting on the ball feeling like my hips were going to rip into two, and getting aggravated that I was going to end up delivering on land again, and I super did not enjoy Aibhlinn’s land birth.
I was helped into the birth pool at 336am, and I was so thankful. I immediately got into the pool, laboring on my knees while leaning over the pool. Time felt so long in this last hour in the pool.

Cullen
At one point, I looked at my IV and could tell it was on the verge of failing. I felt flustered about it, but knew I couldn’t handle for it to be redone at this time in labor and just had to hope and pray the IV would last through placenta delivery and hemorrhage management.
A contraction or two later, Sara could tell the IV was failing, and she was looking at it and looking at my arms and hands. At this point of labor, a lot of things I can’t tell what I was thinking inside versus what I verbalized outside. I know I said something though, and she left the IV alone.

Herbal Bath
I was feeling so much pressure in the pool. The pain was so bad, and I was still unconvinced that the baby was coming. I have never felt so weak in labor as I did this time, and needed Christopher right there to help me with every contraction.
As 4am came, I was prompted to move into semi reclining per my birth preferences. I always had this crazy idea that it would be awesome to catch my own baby, but clearly I am not strong enough in those moments to do it. After being pushed what felt like maybe too much, I moved. I immediately hated that position, but was too weak to be able to move back. I will never deliver in semi reclining again. I give that position zero out of five stars. My pubic bone killed me for weeks after that!

I was assessing his vitals for myself.
The pressure was building, and I felt like he had to be right there but I couldn’t tell. My body started taking over was pushing him down with contractions at 418am. No one was communicating with me, and I couldn’t tell if baby was right there or if someone was going to catch the baby. I know I was being super intense right before delivery because no one seemed ready, and I was scared he was going to come and no one catch him. I asked Rowan what felt like a dozen times if she was ready, and I am sure she was exasperated with me asking. I particularly love this picture Stephanie got of Rowan, Amy, and Jessica all looking to see if baby was right there.

Amy doing Cullen’s newborn assessment.
All of a sudden he was there, and in classic fashion I screamed from the burn of his head crowning. He crowned for what felt like forever before the fetal ejection reflex kicked in, and he came bursting into Rowan’s hands. He was screaming once he came up from water, and proceeded to cry and scream the first hour, making it clear his lungs were in good working order.
I have a favorite video that Christopher took right after he was born because I can see Rowan’s hands dipping into the vernix. When Rowan was my apprentice, she was notorious for trying to get a hold of any loose vernix to put on her wrinkles, and I knew immediately from her hand motions what she was doing.
Thank God this boy was finally here. Cullen Findlater Stellhorn was born on Sunday, September 6th, 2020 at 428am weighing 5lbs 3ozs, finally coming after almost 18 hours of active labor and 10 minutes of pushing. Cullen’s active labor was longer than my three previous active labors combined.

My little helper helping to dress and diaper Cullen.
Sara immediately started running my pitocin, and once I moved to bed, Rowan went to work for placenta delivery. I still had a hemorrhage but nothing at all compared to Aibhlinn’s birth. I got the full package of hemorrhage medications plus a bag of pitocin, which my IV lasted for Sara to push that bag through and then promptly failed. God is so good.
I am thankful for each and every member of my birth team, and thankful they stuck with me through the journey even though it was just as exhausting and tiring for them.
I had so many moments in the late first and second trimesters where I didn’t know how I could go on another day or how September would ever get here as Hyperemesis took over every aspect of my life. I am so thankful for my husband for caring for me and encouraging me through so many bad days, and for the gift God has given us in Cullen. He is an utter delight, and I can’t imagine life without him. He was worth every terrible day of pregnancy.
Love and Gratitude to my Amazing Birth Team:
My midwife, Rowan Twosisters and her assistant, Mary Bratcher, of Preggers Can Be Choosers.
My second midwife, Amy Embrey and her assistant, Sara Escamilla, of Little Love Midwifery.
My doula, Jessica Gonzales, of Village Birth & Babies.
My birth photographer, Stephanie Shirley, of Stephanie Shirley Photography.
To watch my birth film made by the talented Stephanie Shirley, you can watch that here.
As a side note, it was a special blessing to me to have my past apprentices (Rowan and Amy) who were now licensed to be by my side as midwives in my birth. Because of my personality and how particular I am, they got me on that and I had peace that things would go the way I needed them to go with them as my midwives. It was definitely a special moment for me to have two people I participated in their training to be there with me.
 Gwendolyn’s journey from creation to earth side is one full of many unexpected moments ending with one of my most peaceful birthing journeys.
Gwendolyn’s journey from creation to earth side is one full of many unexpected moments ending with one of my most peaceful birthing journeys. Training went from barely bearable to brutal on me while in the throws of the first trimester. I quickly entered horrible aversions and being very rural and far from groceries or restaurants, it was hard to keep me hydrated. My good ole friend Coca Cola actually made me throw up… and it was then I knew this could be bad. I became severely dehydrated suffering from awful dizzy spells, and having to miss sessions because I couldn’t see straight or handle sitting upright. Christopher ended up finding a mobile IV clinic that would come far away for me, and I received fluids and a Meyers infusion and felt some relief. I wish we had found them sooner!
Training went from barely bearable to brutal on me while in the throws of the first trimester. I quickly entered horrible aversions and being very rural and far from groceries or restaurants, it was hard to keep me hydrated. My good ole friend Coca Cola actually made me throw up… and it was then I knew this could be bad. I became severely dehydrated suffering from awful dizzy spells, and having to miss sessions because I couldn’t see straight or handle sitting upright. Christopher ended up finding a mobile IV clinic that would come far away for me, and I received fluids and a Meyers infusion and felt some relief. I wish we had found them sooner!
 We had the name Gwendolyn Elspeth picked out since February of 2019, when we had been to Scotland on holiday. We had been walking in the village of Gullane and passed “Gwendolyn Lane”, and both said that if we ever had another girl, that would indeed be her name. Gwendolyn is Welsh and means fair or blessed, and Elspeth is Scottish and means chosen by God… which for us means our little blessing given perfectly for us from God.
We had the name Gwendolyn Elspeth picked out since February of 2019, when we had been to Scotland on holiday. We had been walking in the village of Gullane and passed “Gwendolyn Lane”, and both said that if we ever had another girl, that would indeed be her name. Gwendolyn is Welsh and means fair or blessed, and Elspeth is Scottish and means chosen by God… which for us means our little blessing given perfectly for us from God. I had my first prenatal visit here in Scotland at 25 weeks. My prenatal care experience was less than ideal and stressful. The community midwife for our village was quite young and seemed very green, and I couldn’t tell from appointment to appointment what was actually going through her mind. It was frustrating to me to constantly hear “NHS protocol” as the response to everything. Within the same appointment, I was told I needed a growth scan because my baby’s are too small, and then when my fundal height was measuring larger than expected, I was told my baby was too big, even with all the valid arguments presenting to her of why mine is larger, she continued with “NHS protocol” information. I refused, and got the lovely risk factor of “care outside of guidelines”.
I had my first prenatal visit here in Scotland at 25 weeks. My prenatal care experience was less than ideal and stressful. The community midwife for our village was quite young and seemed very green, and I couldn’t tell from appointment to appointment what was actually going through her mind. It was frustrating to me to constantly hear “NHS protocol” as the response to everything. Within the same appointment, I was told I needed a growth scan because my baby’s are too small, and then when my fundal height was measuring larger than expected, I was told my baby was too big, even with all the valid arguments presenting to her of why mine is larger, she continued with “NHS protocol” information. I refused, and got the lovely risk factor of “care outside of guidelines”. The community midwife for my village was moving to Glasgow so came to do my “home visit” at the very end of July so it was complete. I was just getting my birth pool and supplies in so it was nice to be getting all the supplies and getting things situated and ready for what we hoped was a late August birth.
The community midwife for my village was moving to Glasgow so came to do my “home visit” at the very end of July so it was complete. I was just getting my birth pool and supplies in so it was nice to be getting all the supplies and getting things situated and ready for what we hoped was a late August birth. We arrived at unit in the early afternoon, and found I was indeed 3cm as I had suspected. I requested steroid injections for the baby’s lungs, and the consultant happily obliged. The midwife and consultant there initially were quite lovely. It was decided I should stay and see what happens.
We arrived at unit in the early afternoon, and found I was indeed 3cm as I had suspected. I requested steroid injections for the baby’s lungs, and the consultant happily obliged. The midwife and consultant there initially were quite lovely. It was decided I should stay and see what happens. I continued with my pacing and showering until the hour passed. He phoned again and was told that the unit was completely full plus it was now shift change, to give it another hour and see what they could arrange.
I continued with my pacing and showering until the hour passed. He phoned again and was told that the unit was completely full plus it was now shift change, to give it another hour and see what they could arrange. I worked my way out of the bath as Christopher made space for the pool in the tiny bedroom that we had planned to place it in. I worked on setting up supplies for the birth as I could between contractions so that everything needed to make things safe was out and available.
I worked my way out of the bath as Christopher made space for the pool in the tiny bedroom that we had planned to place it in. I worked on setting up supplies for the birth as I could between contractions so that everything needed to make things safe was out and available. I labored on my knees in the bed, leaning over the birth ball while waiting for the pool to finish filling. Someone offered for Aibhlinn to come play at their house, so the house was soon quiet and able to just be in the zone. (Aibhlinn has such fun memories of this day, where she left to play with her friend Toby and came home to a baby!)
I labored on my knees in the bed, leaning over the birth ball while waiting for the pool to finish filling. Someone offered for Aibhlinn to come play at their house, so the house was soon quiet and able to just be in the zone. (Aibhlinn has such fun memories of this day, where she left to play with her friend Toby and came home to a baby!) Christopher was a tad anxious and had already been talking to my midwife friend, Rowan, the past few days about things. Once it got passed 11, I told him she may be awake and he could text her if he needed to. She responded and agreed to watch things virtually and guide him accordingly. He had found an old ring doorbell camera that he set up in the room so she would watch from Houston. Still so funny and entertaining.
Christopher was a tad anxious and had already been talking to my midwife friend, Rowan, the past few days about things. Once it got passed 11, I told him she may be awake and he could text her if he needed to. She responded and agreed to watch things virtually and guide him accordingly. He had found an old ring doorbell camera that he set up in the room so she would watch from Houston. Still so funny and entertaining. Time passed… I would move and alternate my position as suggested of me. Everything felt awful. I had already made up my mind that I would deliver semi reclining to make it easier for Christopher to help me even though the recovery last time from it was so awful. So that was a constant thought in my brain through the contractions to be sure I was in that position.
Time passed… I would move and alternate my position as suggested of me. Everything felt awful. I had already made up my mind that I would deliver semi reclining to make it easier for Christopher to help me even though the recovery last time from it was so awful. So that was a constant thought in my brain through the contractions to be sure I was in that position. I could feel Gwendolyn shifting and moving, and the slow build of tiny peaks of pushy pressure trying to start. My body wanted to push, but I wanted to let it build until all my body could do was push.
I could feel Gwendolyn shifting and moving, and the slow build of tiny peaks of pushy pressure trying to start. My body wanted to push, but I wanted to let it build until all my body could do was push. This photo is one of my all time favorites… I had a birth in 2013 where a photographer captured a similar photo at the birth, and I always wished to have one at my own birth. I am so grateful that this photographer got such a beautiful shot.
This photo is one of my all time favorites… I had a birth in 2013 where a photographer captured a similar photo at the birth, and I always wished to have one at my own birth. I am so grateful that this photographer got such a beautiful shot. Welcome to the world Gwendolyn Elspeth, born August 10th, 2023 at 1428 weighing 5lbs 2ozs, 17.75in long.
Welcome to the world Gwendolyn Elspeth, born August 10th, 2023 at 1428 weighing 5lbs 2ozs, 17.75in long. Once the big mess was cleaned up and baby’s blood sugars were stable, we phone the midwives who did not want to come and wanted us to go to the hospital. I informed them I would not be bringing a well newborn with no signs of respiratory distress or other issues to the hospital. They arrived 30 minutes later.
Once the big mess was cleaned up and baby’s blood sugars were stable, we phone the midwives who did not want to come and wanted us to go to the hospital. I informed them I would not be bringing a well newborn with no signs of respiratory distress or other issues to the hospital. They arrived 30 minutes later. It was by far my most peaceful birth. I never would have thought I would have had a free birth, but circumstances pushed us into that situation that we felt absolute peace, and I am certain that if another baby was born here in Scotland, I wouldn’t hesitate to have a similar journey again.
It was by far my most peaceful birth. I never would have thought I would have had a free birth, but circumstances pushed us into that situation that we felt absolute peace, and I am certain that if another baby was born here in Scotland, I wouldn’t hesitate to have a similar journey again.

 S and C started care with me in the first trimester of their third pregnancy. They had their previous babies at home with me, and were looking forward to another home birth journey. You can read about their previous journey’s
S and C started care with me in the first trimester of their third pregnancy. They had their previous babies at home with me, and were looking forward to another home birth journey. You can read about their previous journey’s  Welcome to the world, Adalynn! Born earthside on December 23rd, 2019 at 609am, weighing in at 7lbs 8ozs, 20 inches long.
Welcome to the world, Adalynn! Born earthside on December 23rd, 2019 at 609am, weighing in at 7lbs 8ozs, 20 inches long.